
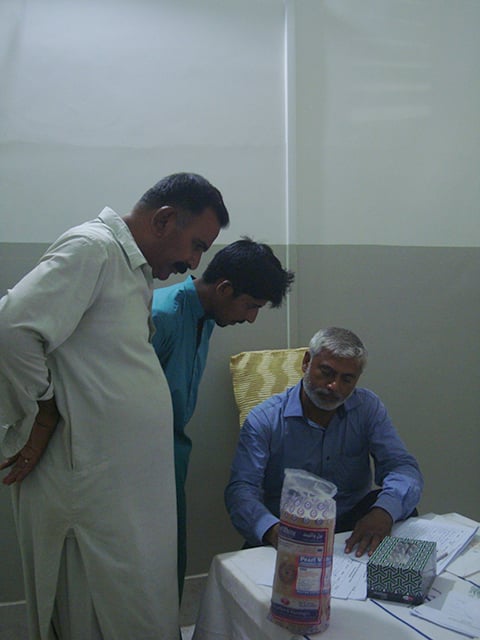
At a 30-minute drive from main Larkana city, an HIV screening camp has been set up in the dusty, minimally equipped, understaffed Taluka Headquarter (THQ) Hospital Ratodero. Hundreds of people are in queue to get tested voluntarily, after watching news on television about the recent HIV/AIDS outbreak in the area. The Sindh AIDS Control Programme (SACP) undertook a mobilisation campaign with the help of the Sindh Health Department, Lady Health Visitors and local representatives of political parties to get people to have themselves tested. Free-of-cost HIV tests are currently being carried out using Rapid Diagnostic Test (RDT) kits, with results available in under 30 minutes.
Till the filing of this report, 19,081 people had been screened, with 617 of them testing positive for HIV, according to the director general of Sindh Health Services. The latest outbreak is unprecedented because it involves the general public — predominantly young children — who do not fall under the high-risk group for the deadly viral infection. Many of the children who tested positive do not have HIV-positive parents. The age group distribution among the reported HIV infections reveals that the most affected age group is two to five years (55.4 percent) followed by six to 15 years (18.8 percent), 15 to 45 years (15.5 percent) and 46 years and up (2.4 percent). Most of the children were screened at the tertiary care facility which is struggling to cope with visitors.
The small town of Ratodero — with a population mostly from the lowest socio-economic segment and comprising of Sindhi, Balochi and some Saraiki speakers — is in panic mode. The numbers at the screening camp have been increasing thanks to word-of-mouth publicity and the fact that hundreds of parents were regular visitors to the clinic of an HIV-positive doctor accused of spreading the infection to thousands of unsuspecting men, women and children.
Charging Rs30 per patient, the accused doctor was the number one choice of many parents because ‘he paid attention to their children’ and was ‘not expensive’. Anaemia, pneumonia, diarrhoea, persistent fever and cough were just some of the ailments that took the poor and, in some cases, well-to-do patients to him. He was also one of the doctors posted at the THQ Hospital Ratodero as a pediatrician.
It took seven deaths — the youngest victim just seven months old — and a brave father’s use of social media to highlight Ratodero’s HIV/AIDS outbreak. And what has happened in the subdivision of Larkana, Sindh, since April 23 has grabbed the attention of national and international media. This also led to the doctor’s arrest. A three-member technical team has submitted a detailed report to the JIT investigating the doctor, who has already been demonised in the media.
The HIV/ AIDS outbreak in Sindh, primarily among children, has rightly sent shockwaves across the country. But the sensationalist headlines and demonisation of one doctor mask the underlying issues of poor priorities and the hydra-headed predicament of healthcare in the province...
Allah Dino, a resident of Ratodero, is at the camp to get tested with his wife and four children. Though he says he has never indulged in extra-marital sex or drugs, Allah Dino feels the tests are needed. “My wife’s last two births were painful and she needed a blood transfusion,” he says. She hasn’t been keeping well for months now.” An hour later, he walks away happily from the camp; his entire family tested negative for HIV. A doctor guides him to get his wife tested for tuberculosis (TB).
Meanwhile, a young father from a nearby goth stands clutching the lab report of his two-year-old son in one hand and protectively holding the boy in the other, and looking visibly upset. “Everyone from my village is getting tested and I thought of getting my son tested, too,” he says. “I had taken my son to the same doctor. Since his arrest I have been very upset and took my son for an HIV test.” The test, taken at the People’s Private Health Initiative (PPHI) lab, confirmed the boy was HIV-positive. “I want to reconfirm this,” he says. After an agonising wait of some 40 minutes, the RDT test also comes back positive. The staff guides him to take his son to Larkana, assuring him the boy would be fine once treatment begins. “He will go on to have a wife and kids,” says a volunteer, trying to reassure the father.
Talking to Eos, Nazeer Hussain, the father of an HIV-positive toddler, says had it not been for social media, no one would know what was happening in Ratodero. Since April 23 onwards, his Facebook page has been littered with posts aimed at raising awareness about HIV and his activism is earning him support from the parents of other HIV-positive children.
“My child was ill for months and I took her to various doctors including [the accused]. After months of treatment, she was still unwell and that is when Dr Imran Akbar Arbani [a friend of his] said I should get an HIV test done.”
Hussain says he was horrified and angry at the mention of an HIV test for his child but eventually agreed. “When I saw the positive report, I felt the world around me crash.” The positive report prompted Dr Arbani — a joint Guinness World Record holder for removing the heaviest kidney stone — to suggest more children be screened. By the end of April, he had access to reports of over 80 confirmed cases, including those of the seven deceased. This is when calls were made and the District Commissioner Larkana forced the accused doctor to take the test. It turned out positive much to the shock and dismay of the families and the doctor himself.
At A Loss For Words
A visit to the crowded first floor of Larkana’s HIV/AIDS Treatment and Care Centre of the Chandka Medical College (CMC) Hospital is an eye-opener. The lobby teems with anxious parents — most mothers holding on to their children look malnourished. They are accompanied by haggard-looking husbands or in-laws, as they wait for their turn to meet Dr Shehla Baqi, the head of the Infection Control Programme from the Dr Ruth KM Pfau Civil Hospital, Karachi, and the Aga Khan University Hospital’s Paediatric Infectious Diseases specialist, Dr Fatima Mir. The two female doctors make a formidable team along with Dr Holaram Thakuria — the in-charge of the treatment centre handling adult HIV cases in Larkana district since 2005 — and diligently deal with confirmed cases sent their way from Ratodero.
“I have twin boys, one of whom I gave to my sister,” says a young woman in her 20s, waiting for her turn at the CMC Hospital. “I was stunned when I found out that my boy, adopted by my sister, is HIV-positive,” she says. Her sister is also HIV-positive but she is unclear about the status of her brother-in-law. “I hope my son will be fine,” she says.
Healthcare providers and volunteers from the camp and the hospital note that the biggest challenge is people not having a record of their children’s medical history.
A volunteer at the HIV centre blames lack of education and lack of awareness among the people. “They have no idea what they are dealing with, [there is] too much misinformation. Some believe the polio vaccine is behind this outbreak, others feel the water supply is contaminated with the virus. Then, there is this misconception that sharing utensils at tea shops might be the cause.
“There is awareness that sharing razor blades can cause infection but people don’t realise that the tools used for circumcision also need to be sterilised or blood transfusions should be safe,” he says. “Usually, dispelling myths around HIV/AIDS requires a lot of counseling for an HIV-positive individual, but what we are seeing here is unprecedented. I am at a loss for words,” the volunteer adds.
DOCTOR AT THE EYE OF THE STORM

Meanwhile, the case of the accused doctor is not as cut and dried as presented by the media.
Under Article 19 (1) of the Sindh HIV and AIDS Control Treatment and Protection Act, 2013, “No person shall be compelled to disclose HIV-related information or any other private information concerning himself, except when a court determines by an order that the disclosure of such information is necessary for the determination of issues and in the interest of justice in a matter before it.”
The Sindh government has sent yet another blood sample of the accused — obtained under duress according to the accused as well as multiple sources — to the Aga Khan Hospital, results of which are still awaited.
Though the findings of the technical team are not public, the members and other infectious disease experts conjecture that the current outbreak is ‘multifactorial’ (especially genetic or environmental factors). Experts think it unfair to make one man a scapegoat for this epidemic which spiralled out of control due to poor infection control practices and general apathy on the part of the government.

Dr Anila Isran, the Women Medical Officer and Coordinator of Prevention of Parent to Child Transmission (PPTCT), HIV Treatment Centre, Sheikh Zayed Women Hospital in Larkana, has been caring after HIV-positive women since 2011, when the centre was launched at the facility. “The total number of registered cases with me is 102 right now,” she says. “Most women who come for consultation have no idea about the disease and are very vulnerable. They usually get the HIV infection from their husbands.” She adds that injections and blood transfusions are the other causes.
Hussain, a barber and a father of nine, says his five-year-old son tested positive for HIV. “I found out some seven months ago after I took my wife and son to the doctor’s. The two had been ill for months,” he says. His wife was given a blood transfusion. The man who donated his blood was an acquaintance of his nephew.
Iron-deficient anaemia and post-partum hemorrhaging are often the reasons why women require blood transfusions — with no guarantee that the units have been screened.
After months of illness, his wife tested positive for HIV. “Dr Holaram told me to find the man who donated the blood, saying his life may be in danger. When we went to his house, we found out he had passed away last year due to a protracted illness.” Since then, the deceased’s family has been tested for the infection. They were safe from the life-threatening disease but not from the community backlash.
Meanwhile, Hussain’s test came back negative. Though his family never visited the accused doctor, Hussain says the government must take notice of this injustice and hold everyone involved accountable, including blood banks.
Over a dozen parents interviewed by Eos, at various health facilities and the screening camp at THQ Hospital Ratodero, said they never took their children to the accused doctor. The interviews were also corroborated by health care providers at the screening camps.
“Since the outbreak, I have seen women walk in more frequently at the hospital. Earlier, it would be a woman every few months but, in the past 10 days, I have seen eight cases. One woman each is from Shikarpur and Dadu while the remaining cases are from Ratodero,” says Dr Isran.
Urging for more screenings and awareness, Dr Isran says a lot of work needs to be done to raise awareness to save women and thereby their babies from HIV.
What Went Wrong?
According to the UNAIDS 2017 factsheet, Pakistan is home to an estimated 150,000 HIV-positive people, with some 3,500 under the age of 14 years. 22,000 Pakistanis living with HIV know of their status while only 12,000 are currently on antiretroviral therapy (ART). The national and provincial AIDS control programmes say the actual numbers of people with HIV is likely much higher.
Since the first reported case of HIV in 1987 in the country, the epidemic took root mainly in high-risk populations — drug users and sex workers — as well as migrant workers in the Gulf deported back to Pakistan once their HIV-positive status was known. A poor health care system, and social stigma made talking about HIV a taboo, however.
The HIV epidemic in Larkana district is also not a new one. The first HIV case was reported there in 1995. Eight years later, in 2003, the city garnered attention when the first outbreak of HIV among injecting drug users (IDUs) was reported. Out of 175 IDUs, 17 were confirmed positive. A paper titled “Alarming Increase in Reported HIV cases from Larkana, Pakistan: A Matter of Serious Concern,” published in the Journal of the Pakistan Medical Association in 2014, notes:
“In 2008, results of … national surveillance suggested 27.6% hijra [sic] sex workers were confirmed HIV positive. This [Larkana] has to be a unique town in Pakistan because of an unusual pattern of multiple commercial sex activities happening here. It has a functioning brothel where clients from all over the district as well as from the other cities visit female sex workers in [the] daytime for commercial sex. Additionally, there are home-based sex workers as well, who [see] clients on [a] regular basis. There are at least two musafirkhanas [motels] on Station Road in the middle of the city where hijra [sic] and male sex workers are available round the clock to provide paid sex services to clients.”
The report goes on to add that the city has all the ingredients of an exploding HIV epidemic in the near or distant future.
That prediction came true in 2016 when a hemodialysis-unit-related outbreak in Larkana made headlines and the number of HIV-positive people in the district crossed the 1,200 mark. With HIV present in a high-risk population — comprising of IDUs, female sex workers, transgender sex workers and men who have sex with men — for around two decades, and with unregulated blood banks, the rampant reuse of unsterile syringes, rudimentary healthcare facilities, poor infection control practices and untrained healthcare workers, the infection finally made its way to the general public.
“HIV/AIDS was never considered an emergency or a big issue,” says Dr Sikandar Memon, programme manager of the SACP. “This is a very small programme going nowhere. When there are so many unsafe practices all over the country, anywhere you test you will end up getting some HIV-positive people.”
He says that, despite funding crunches, the SACP has been working diligently with high-risk groups. “But we don’t have enough resources or the mobilisation capacity to reach the general public.”
So how high is the provincial AIDS control programme on the list of the Sindh government’s priorities?
In terms of response, it took the Sindh Health Minister Dr Azra Pechuho 20 days to visit the screening camp at Ratodero. In a press conference later that day, she said it wouldn’t have made much of a difference had she visited earlier.
According to sources, the PC-1 budgetary allocation for SACP was earmarked at Rs1,623m for a period of three years (2016-19). The budget was released in 2017 and so far only Rs211m has been disbursed. Then, when the programme made a request for Rs38 million for RDT kits for the ongoing fiscal year it received only Rs4.9m. Since the outbreak, an additional 22.6m rupees have been released. The SACP’s service delivery programme has not been functional since 2014. Only when funds are available are the NGOs and community-based organisations engaged for awareness campaigns.
The SACP has seen its fair share of controversy, too. In July 2018, the executive board of the National Accountability Bureau approved an inquiry against SACP Programme Manager Dr Muhammad Younas Chachar and others for misuse of authority and embezzlement in government funds that allegedly caused a loss of Rs35.236 million to the national exchequer. Chachar retired on January 19, 2019.
Dr Memon became the SACP programme manager on February 6, 2019, after being sidelined as an OSD (Officer on Special Duty) in the provincial health department. Nevertheless, the ongoing screening effort currently underway in Ratodero saw him actively lead his team, along with other stakeholders — a task which is beyond the scope and resources of the SACP.
Under its current strategy, the SACP has taken on board a team of infectious diseases specialists and experts from UNAIDS and the WHO to chalk out a short-term and long-term plan to deal with the HIV outbreak.
Dr Memon urges the government to ensure that the relevant departments work together to deal with this hydra-headed monster. He points out a dire need for collaborative effort. “We have to ensure decentralisation of treatments and testing services, setting up of satellite centres and existing network of public blood banks,” he says. “Strong referral mechanisms between the institutes are needed. Last but not the least, confidentiality of results has to be ensured.”
The Sindh Health Care Commission was established under the Sindh Government Act 2013 for regulating health care services in the province of Sindh. However, the commission obviously failed in keeping a check on healthcare facilities in the province and a tab on quacks. As a knee-jerk reaction after the HIV outbreak garnered news headlines, it had 41 clinics sealed in Larkana and issued notices to 100 medical practitioners for questionable practices.
Under its new head, Dr Durenaz Jamal, the Sindh Blood Transfusion Authority (SBTA) has also sealed some facilities. Furthermore, according to the SBTA, no bloodbank in Ratodero was registered with the authority. “These were small labs that were selling blood to the people without proper screening. There is no awareness amongst the people about safe blood and these labs were exploitative. This amounts to quackery,” says Dr Jamal. She adds that the SBTA always encourages establishing new blood banks, but only those which work according to its criteria and operating procedures.
Stepping up efforts

Infectious diseases experts say that this outbreak could have been prevented had proper systems been in place. “You have a population which is vulnerable, faces poverty, illiteracy, malnutrition and now has a chronic illness,” notes one expert.
“The government needs to focus on why the situation got out of control. The people have poor understanding of the disease and treatment could be jeopardised. The efforts shouldn’t just stop at screening,” says Dr Bushra Jamil, head of Infectious Diseases at Aga Khan University.
Meanwhile, SACP’s Dr Memon stresses that HIV-positive adults and children can go on to live ‘healthy, happy lives’ as long as they follow the ART regimen religiously. “These children will grow up to be fine adults, with no complications. They can work full time and marry and contribute positively to the society.” The key, he stresses, is to “ensure these men, women and children take the medicines regularly”.
Dr Jamil is not so sure. “How can we ensure that lifelong treatment is religiously followed? The virus becomes resistant if treatment is interrupted and then becomes difficult to treat.”
She urges the provincial and federal government to create awareness about not giving unnecessary injections (unless life-saving) to infants and children. “There is a need to maintain strict safety and hygiene protocols and availability of screened blood for transfusions,” she adds.
Dr Syed Faisal Mahmood, assistant professor of adult infectious diseases at AKU and member of the response team which visited Ratodero to assess the situation, says infection control interventions are needed immediately: “Hand hygiene facilities or disposal and use of sharps [sharp instruments]are suboptimal and not as high a priority and often thought of as distinct from the routine medical care of prescribing medications or running tests. Again here, hospital administrations need to play a key role.”
A 2018 study “Reuse of Syringes for Therapeutic Injections in Pakistan: Rethinking its Definition and Determinants” notes that “Frequent reuse of syringes during medical injections is fuelling HIV and Hepatitis C (HCV) epidemics in Pakistan.” The study further points out that, “A rural location and longer duration of practice predict a higher likelihood of reuse. Physicians and non-physicians were equally likely to reuse. Most patients were unaware when a syringe had been reused.” It concludes that “very high syringe reuse is driven by high injection demand by patients, to which providers comply. Patients are generally unaware of the harm of injections and syringe reuse or that reuse happens.”
Dr Sunil Dodani, assistant professor at Infectious Diseases, SIUT, says that blanket ban on sale of reusable syringes or closure of blood banks doesn’t help much. “There needs to be a concentrated effort to ensure availability of sterilised syringes and tools. People must be made aware that unnecessary injections must be avoided.” He also stresses the need for safe disposal of infectious waste by municipal corporations, ideally through incinerators or marking sites for landfill.
“Most importantly, the government needs to ensure that hospital waste disposal mechanisms are functional,” he says.“You will have to discard a used auto-lock syringe too. Unless you don’t have proper waste disposal mechanism, this will remain a problem.”
The results of the epidemiological investigation into the HIV outbreak in Ratodero will be available in a few months from now and will eventually allow the government and all stakeholders to come up with a long-term strategy. So far, the patients declared HIV-positive after screening are being interviewed at CMC hospital to obtain the details that led to the infections — in most cases it seems to be the result of reused injections, followed by unsafe blood transfusions.
The SACP and the Sindh Health Department have yet to make a prediction about the number of cases they will be dealing with in the near future, at a time when some 50 people are being added to the list on a daily basis. However, at this critical juncture, the Sindh government must ensure the availability of safe blood, sterile syringes and proper medical waste disposal mechanisms, while ensuring that medical requirements of the affected are taken care of and privacy of all individuals caught in this crisis is respected.
The writer is a member of staff.
Why we need to talk about HIV/AIDS
HIV stands for human immunodeficiency virus. HIV attacks and destroys the infection-fighting CD4 cells of the immune system. The loss of CD4 cells makes it difficult for the body to fight infections and certain cancers. Without treatment, HIV can gradually destroy the immune system and advance to Acquired Immunodeficiency Syndrome (AIDS), the most advanced stage of HIV infection. Though there is no cure available for HIV as of now, antiretroviral therapy (ART) can treat the HIV infection, allowing people with the illness to live healthier lives as well as reduce the risk of HIV transmission. The latest research says an undetectable viral load — when one is regularly taking HIV treatment (ART) — also stops HIV transmission (also known as U=U: Undetectable = Untransmittable).
Responding to Eos via email, UNAIDS Country Director Pakistan and Afghanistan Dr Maria Elena G Filio Borromeo says, UNAIDS, UNICEF, the WHO and other partners are working closely with the Sindh Ministry of Health to address the acute needs of the people infected with HIV and to support an outbreak investigation. “The findings and recommendations from this investigation will help shape and inform the appropriate measures that need to be implemented, both in the short and long-term. These measures could include banning of unsafe injection and blood transfusion practices, wide dissemination of correct information about HIV/AIDS and related issues in the community, enhancing capacities of health workers in providing voluntary counselling and testing, addressing stigma and discrimination which often leads to prejudice, and mobilising domestic resources to sustain the response.”
Urging for enhanced awareness and destigmatisation, she notes that — unlike other infectious diseases — AIDS is associated with behaviours that are not often acceptable in most societies, particularly in Asia. “Prejudice and rejection could kill people living with HIV faster than the virus itself,” she says. “In addition, women and children have limited access to quality health services because of their socio-economic status in the society. Biologically also, women — particularly young women — face higher vulnerability to HIV and other sexually transmitted infections.” — S.J.
Published in Dawn, EOS, May 26th, 2019














































Dear visitor, the comments section is undergoing an overhaul and will return soon.