
My eldest sister’s servant got the flu recently. He had a cough, runny nose and low-grade fever and was unable to cook. She asked him to take some medicine, including an antibiotic, which he did for a few days, until his symptoms settled.
It seems a simple enough remedy, but I believe she made a mistake. Can you guess what it was?
The irrational, indiscriminate and excessive use of antibiotics, including self-medicating with them, increases antimicrobial resistance and, at times, creates poor or no response to antibiotics.
The main cause of antibiotic resistance is antibiotic use. When we use antibiotics, some bacteria die but resistant bacteria can survive and even multiply. The overuse of antibiotics makes resistant bacteria more common. The more we use antibiotics, the more bacteria are likely to become resistant to them.
The first antibiotic, Salvarsan, was introduced in 1910 in treating conditions like syphilis. In just over 100 years, antibiotics have drastically changed modern medicine and extended the average human lifespan by 23 years. The discovery of penicillin in 1928 by Alexander Fleming, which began the era of antibiotics, has been recognised as one of the greatest advances in therapeutic medicine.
But approximately 700,000 people die across the world each year now due to drug-resistant infections, with the potential of this number rising to 10 million by 2050, unless action is taken. The number of antibiotic resistance-related deaths in Pakistan is higher than deaths from cancer, respiratory infections and tuberculosis, typhoid, diabetes and kidney diseases, and chronic respiratory diseases.
The over-prescription by doctors of antibiotics for minor illnesses and people’s reliance on self-medication and unqualified health practitioners is leading to a dangerous rise of drug resistance in Pakistan
According to a local study involving 480 participants, 34.2 percent had used prescription antibiotics, 32.5 percent had self-medicated and 33.3 percent could not remember. The prevalence of self-medicating with antibiotics was higher in men and the highest prevalence was noted among age groups of 31–40 years old (15.4 percent).
These results showed that 35.4 percent of participants did not see doctors because they said they did not have the time, while 15.2 percent said that they did not do so because they did not have enough money for a doctor’s visit. Meanwhile, 8.1 percent implicitly said they do not trust doctors.
According to research in Pakistan in 2020, an overwhelming 96.9 percent of pharmacies and medical stores administered antibiotics without requiring a prescription, encouraging antibiotic overuse, self-medication and antimicrobial resistance. According to another study from Pakistan, 78 percent of antibiotics are prescribed for mild illnesses. Misuse or overuse of antibiotics are leading to drug resistance, but many antibiotics have also developed multi or extreme drug resistance.
One reason for the overuse of antibiotics is people’s reliance on pharmacists and quacks for medical advice. They, in turn, pose as general practitioners and dole out advice they are not trained to give, and prescribe medicine or syringes they are not qualified to.
Ignorance and poverty have contributed towards the survival of quackery in Pakistan. People from rural and remote localities, due to a lack of awareness and limited exposure, are clueless about the definition of a doctor and the functioning of a medical facility. The latest healthcare census found Punjab, Pakistan’s most populous province with 110 million inhabitants, to have between 70,000 and 80,000 unqualified medical practitioners.
But qualified general practitioners (GP) are also in the habit of relying on antibiotics.
One study found GPs in Pakistan prescribed at least one antibiotic in 62 percent of prescriptions, compared with specialists who wrote one antibiotic in 54 percent of their prescriptions. Over 48 percent of GP prescriptions had at least one injectable drug, compared to 22 percent by specialists. Thirteen percent of GP prescriptions had two or more injections.
Doctors say they are compelled or forced to prescribe an antibiotic even if the patient does not require it. They cite some of the reasons as pressure from the patients or their families, and time constraints and uncertain diagnoses, ie being unable to differentiate between a person who has viral or bacterial infection as they often have similar symptoms. In such a case, a doctor may go ahead and prescribe antibiotics.
But there are severe risks involved for those who self-medicate using antibiotics. The first is incorrect self-diagnosis, along with potential adverse reactions to the medication. Then there is the risk of a worsening of the condition of the patient seeking to treat themselves. There’s also the possibility of the masking of severe diseases, dangerous drug interactions and the risk of dependence and abuse.
People turn to the following the most when self-treating: antipyretic (100 percent), antibiotic (80.4 percent) and vitamins (59.9 percent).
The example of a male doctor who got diarrhoea should serve as a good example of drug resistance. His doctor wife prescribed him an antibiotic for five days but he only took it for two days because his diarrhoea had stopped. Even though he is a doctor, he did not realise he was creating drug resistance by leaving his treatment incomplete. While he was cured within a few days, should his ailment return and he has to take antibiotics again, he may find it longer to get better next time, or find the antibiotic doesn’t work as well.
Incomplete knowledge and misperceptions about the use of antibiotics and the subsequent consequences of their misuse must be highlighted to successfully tackle the issue. Health professionals can play a vital role in prevention, by educating people about the potential risks of antibiotic use as people are more likely to trust and consider their therapeutic advice and medical knowledge.
When a patient is diagnosed with an infection that needs to be treated with antibiotic drugs, the medical professional should provide proper instructions on their usage, such as dosage, frequency of doses, the length of the treatment course and the harmful effects of their misuse.
Hospitals and big clinics should implement “Antibiotic Stewardship Programmes” to train doctors and nursing staff, especially in critical care units, to prevent the spread of resistant bacteria.
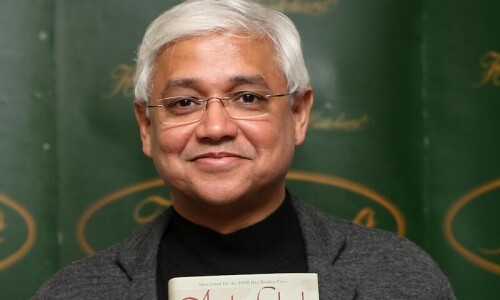
The writer is medical director at Shine Humanity and can be reached at asghar.naqvi@shinehumanity.org
Published in Dawn, EOS, January 21st, 2024












































Dear visitor, the comments section is undergoing an overhaul and will return soon.