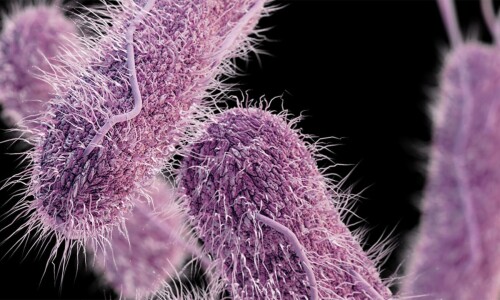
WHO would have thought that the medicine that was developed to cure disease would one day be overpowered by the very microorganisms it was supposed to target?
Medical science may have progressed with lightning speed over the decades, but has now hit a significant roadblock in the form of antimicrobial resistance. From Nov 18 to Nov 24 — World Antimicrobial Awareness Week — countries will be reminded of this grim reality, as thousands of people worldwide continue to die because their sickness is not responding to antibiotic treatment.
This should be especially alarming for a country like Pakistan, where the consumption of antibiotics is the third highest in the world. There are no checks on the intake of these drugs, thanks to a general lack of awareness and a lax attitude on the part of doctors, pharmacies and patients. Doctors often recommend antibiotics to patients without even diagnosing their illness; pharmacies readily sell them over the counter, and those consuming them resort to their improper use.
Under these and other circumstances, pathogens develop resistance. Indeed, when in a country like the US, with its high-quality healthcare, almost one-third of antibiotic prescriptions are not needed, one can expect worse in Pakistan, where regulations and international best practices are routinely overlooked.
The situation is nothing less than a medical emergency: between now and 2050, medical experts expect antibiotic resistance to kill 40m people worldwide. A disproportionate number is likely to be from the developing countries where healthcare is poor and disease-rife — a situation that is compounded by high levels of illiteracy and lack of education. Against this backdrop, it would indeed be a miracle if this year’s theme for WAAW — ‘Educate. Advocate. Act now’ is taken seriously by our authorities — not simply for health reasons but also to reduce the huge economic burden caused by longer hospital stays, more expensive, often inaccessible, therapy, and loss of work hours.
A coordinated strategy is needed at a national scale to reduce the microbial danger. But, in the meantime, health authorities can step up disease-reducing measures such as carrying out frequent vaccination campaigns, ensuring cleanliness in neighbourhoods and public places, and keeping a vigilant eye on hospitals — the hotbeds of infection.
As recommended by the WHO, they would do well to promote antimicrobial stewardship to train doctors in judiciously prescribing and administering antibiotics. Besides, affordable lab tests can lead to more accurate diagnoses for patients who are otherwise deterred by high costs. Nothing, of course, can take the place of greater awareness among the public itself. But the state has to lead the way by recognising the health challenge and taking steps where it can.
Published in Dawn, November 18th, 2024









































Dear visitor, the comments section is undergoing an overhaul and will return soon.